Ärzte Krone
Fortbildung, Informationen und Service für niedergelassene Ärzt:innen

Apotheker Krone
Fortbildung, Service und beratungsrelevante Informationen für die Tara

ARZT & PRAXIS
Das Magazin zur Diplomfortbildung in Österreich

AHOP-News
Special-Interest-Medium für hämatologisch und onkologisch tätige Pflegepersonen

DIABETES FORUM
Hot Topics der Diabetologie interdisziplinär und praxisbezogen aufgearbeitet
FAKTEN der Rheumatologie
„Die“ rheumatologische Fachzeitschrift Österreichs zu State of the Art, Wissenschaft und Forschung + jede Ausgabe mit DFP-Beitrag

GYN-AKTIV
Fachmagazin zur Frauenheilkunde für Kliniker:innen und Niedergelassene

NEPHRO Script
Offizielles Organ der Österreichischen Gesellschaft für Nephrologie (ÖGN)
neurologisch
Offizielle Fachzeitschrift der Österreichischen Gesellschaft für Neurologie (ÖGN)
PHARMAustria
Das Branchenmagazin für Führungskräfte und Entscheidungsträger der pharmazeutischen Industrie

Das Medizinprodukt

SPECTRUM Dermatologie
Facettenreiche Dermatologie: chronisch entzündlich, infektiös, onkologisch & mehr

SPECTRUM Onkologie
Aus der Forschung in die Praxis: Die Welt der Onkologie mit ihren vielen Gesichtern
SPECTRUM Pathologie
Pathologie als Weichensteller: Der präzise Blick für die exakte Diagnose
SPECTRUM Urologie
Am Ball bleiben auf einem breiten Themenfeld der Uro(onko)logie
SPECTRUM Psychiatrie
Fokusbezogene, aktuelle Themen aus Psychiatrie & psychotherapeutischer Medizin

Universum Innere Medizin
Streifzug durch die Innere Medizin im offiziellen Medium der ÖGIM

Fortbildung, Information und Service für Zahnmediziner:innen
Austrian Atopy Update
Eine Plattform mit dem Ziel, regelmäßig neue und relevante wissenschaftliche Studien zum Thema atopische Erkrankungen bereitzustellen
car-t-cell
CAR-T-Zellen als Game Changer - kuratives Potential auf hohem Niveau

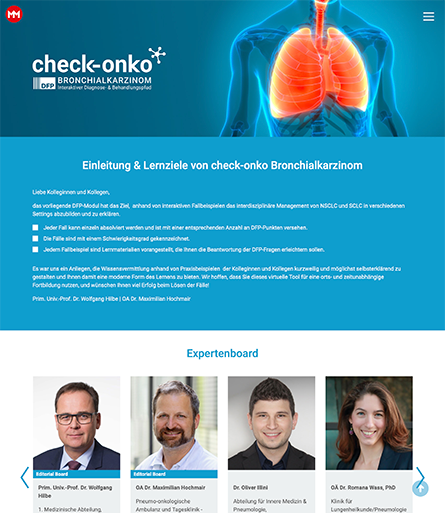
Case Report Interactive
Wissenschaftliche Evidenz und Empfehlungen aus der klinischen Praxis werden anhand eines konkreten Fallbeispiels vermittelt.

congress x-press
Expert:innen berichten Studienhighlights von (inter)nationalen Kongressen via Newsletter

DigitalDoctor
Zielgerichtete Therapie chronisch entzündlicher Dermatosen
derma-target
Das neue Portal für die Medizin der Zukunft

Expertenforum
5 Fragen zu einem Thema werden von 5 Fachexpert:innen beantwortet. Zusammengefasst und kommentiert von einem/einer zusätzlichen Experten/Expertin.
Fast Facts Interactive
Die crossmediale Kombination: komprimierte Key Messages einer Studie plus Infografiken und Animationen
IM FOKUS
Themenchannels mit Qualitätscontent on Demand
krebs:hilfe!
Fachmedium für die bestmögliche onkologische Patientenversorgung

mol-onko
Die Website für zielgerichtete Therapien in Hämatologie und Onkologie
nextdoc
Die Plattform für Jungmediziner:innen

Podcast
Gezielte Information über Produkte, Services für Gesundheitspersonal oder die breite Öffentlichkeit

RELATUS MED
Das Newsportal für Medizin und Gesundheitspolitik

RELATUS PHARM
Das Newsportal für Pharmazie und Gesundheitspolitik
Study Shortcut
Studien durch Animationsvideos leicht verständlich gemacht
Therapie News
Single-sponsored, monothematische Focus-Website
Bücher
Fachbücher mit Fokus Gesundheit verfasst für ein breites Publikum

Gesundheit verstehen
Leicht verständliche und wissenschaftlich fundierte Broschüren
Neue Horizonte
Journal der Österreichischen MS-Gesellschaft
Pocketguides
Alle relevanten Informationen zu einer Indikation, zusammengefasst strukturiert und im handlichen Format

Apps
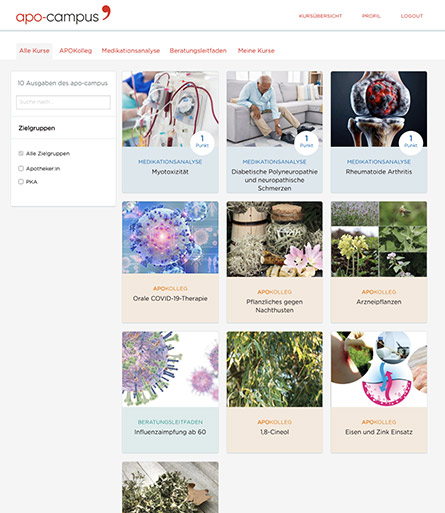
Hier finden sie APPs für medizinisches Fachpersonal supported by MedMedia
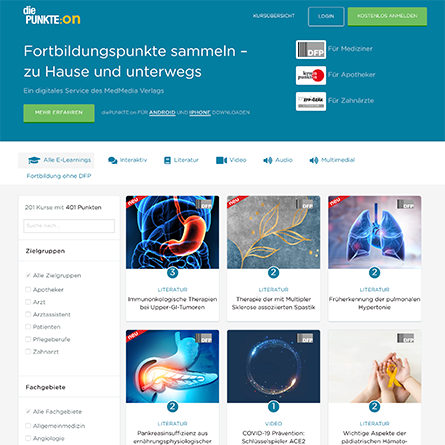
Leistungsbeschreibung und Preise zu unseren MedMedia-Produkten für Print und Digital
Das MedMedia Team: über 60 Mitarbeiter:innen mit medizinischer und pharmakologischer Fachkompetenz
Werde Teil von unserem Team. Erfahre mehr über die Fima und Jobs bei MedMedia
MedMedia Verlag und Mediaservice GmbH
AdresseSeidengasse 9/Top 1.1, 1070 Wien
Telefon:+43 1 4073111-0
Fax:+43 1 4073114
Abonnieren sie hier Fachmagazine passend zu ihren Interessen oder Fachgebieten
Melden sie sich hier für die Newsletter passend zu ihren Interessen oder Fachgebieten an
Neu Registrieren
Ich habe noch kein Benutzerkonto und möchte mich kostenlos registrieren.
Zur RegistrierungThe Relevance of Chronic Inflammation for Genomic Instability in Cancers
Melden Sie sich bitte hier kostenlos und unverbindlich an, um den Inhalt vollständig einzusehen und weitere Services von www.medmedia.at zu nutzen.

Stem Cells and Leukemia Laboratory, University Clinic of Hematology, Inselspital Bern, Bern, Switzerland. Department of Biomedical Research, University of Bern, Murtenstrasse 40, 3008 Bern, Switzerland. Contact

SO 02|2020
Publikationsdatum: 2020-05-04
Zur Ausgabe »